
How joints work
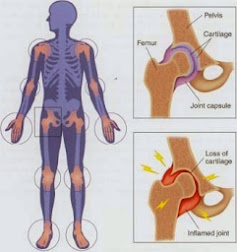
In order to have an understanding of the two major types of arthritis, it is essential to know a little about the function and appearance of a joint. A joint is designed to allow smooth movement of two bones, one against the other.
The essential components of the joint are:
• Ligaments - 'Rope-like' bands that hold the bones together.
• Cartilage - Smooth material that allows one bone to move over the other without friction.
• Synovium - The joint-lining cells that produce a small amount of fluid (like oil) to lubricate the joint.
• Tendons - Inelastic bundles of fibre that attach a muscle to a bone.
The Types Of Arthritis
Osteoarthritis (or degenerative arthritis): Osteoarthritis is the most common form. It occurs when the cartilage of the joint gradually wears away, exposing bare bones that rub against one another. This makes the joints stiff, 'creaky' and painful. As this disease is a 'wear and tear' disease, it tends to occur in older people and those whose joints have been damaged by injury.
Rheumatoid arthritis: Rheumatoid arthritis, on the other hand, is an 'inflammatory' arthritis. The synovium (see above) becomes much thicker and changes its character so that the inflammatory cells within it start to eat away at everything they touch. Joints affected by rheumatoid arthritis often become unstable and slip out of place, causing deformities of the hand, for example. It commonly affects younger women aged 20 to 50 years.
What treatment Is There?
Other medicinal treatments include:
• Non-steroidal anti-inflammatory drugs for osteoarthritis and particularly rheumatoid arthritis. Make sure you take this medication at regular intervals (as advised by your doctor). Potential side-effects of these medications include the development of stomach and duodenal ulcers, although there are some medications designed to reduce this risk.
• Drugs such as sulphasalazine, gold and methotrexate for rheumatoid arthritis. Called suppressive agents, these drugs are effective but have some serious side-effects in some people. They must be closely monitored by your doctor.
• Cortisone injections and cortisone-like tablets (also known as steroids). Their benefits are often dramatic and when used in low doses, are extremely useful in controlling arthritis. The cortisone preparations used for arthritis are not the same steroids used by some athletes.
Exercise and physical therapy
Physical measures such as exercise and physiotherapy are essential to maintain your range of movement in joints and to keep your muscles as strong as possible. A regular exercise programme designed to suit you is an essential aspect of pain management and will enhance your feelings of well being. Occupational therapy is important as it can help your environment become more 'user-friendly'. In other words, aids can be obtained to help you turn on taps, open doors and put on clothing. Also, appropriate, comfortable, supportive footwear (if carefully made) can eliminate pain when you walk.
Can surgery help?
Hip replacement and knee replacement surgery has been one of the major advances in the past 15 years for people with arthritis. These operations are now performed quickly, with short periods of hospitalisation. Although all operations can have complications, problems are becoming less and less common. Surgical correction of foot deformities in rheumatoid arthritis and osteoarthritis is beneficial but as yet not all deformities are correctable, particularly those of the elbows, shoulders and ankles. Ask your doctor if surgery is right for you.
Your state of mind
The development of arthritis can cause depression. You may mourn for your loss of health and become frustrated when performing tasks that were easy before. The lethargy and tiredness common in severe arthritis can make any depression worse.
If you can come to terms with these feelings of depression, the arthritis often becomes easier to manage and certainly easier to live with. To overcome negative feelings, try developing:
• A positive attitude.
• An exercise programme (particularly swimming). Start with an exercise you enjoy and be sure to speak to your doctor before starting a new fitness programme.
• A change of lifestyle, including a sensible diet to control your weight (reducing the load on damaged joints).
• A pain management plan that will help you learn how to manage pain and stress in a positive way.
• A sympathetic and supportive family and doctor can be of great value too.
What about 'alternative' remedies?
When it comes to the treatment of arthritis, everyone seems to have a 'pet cure'. These cures vary from naturopathy, homoeopathy and dietary restrictions to massage and chiropractic. Virtually all patients who develop arthritis will try one or more of these remedies looking for a miracle cure.
Miracle cures are rare indeed and there is very little scientific evidence to back these forms of therapy. However, it is also fair to say that in the majority of cases these forms of therapy are not harmful. A good nutritious diet, a regular massage and some vitamin supplements may well make you feel better even if they rarely cure arthritis.
By Dr Neil Munro, FRCGP.

















No comments:
Post a Comment